Analgesic treatment is a vital aspect of veterinary medicine, and the use of analgesics is essential to providing high-quality medical care to animals. In addition to preoperative anesthesia planning, regional anesthesia/analgesia is an important component of balanced anesthesia in veterinary medicine. Regional pain relief involves using local anesthetic medications to block specific nerve pathways in specific areas of the body.
Regional anesthesia plays a vital role in balancing anesthesia in veterinary medicine. It offers several advantages over general anesthesia, including better pain control, reduced risk of complications, and faster recovery time. Regional anesthesia may be used alone or in conjunction with general anesthesia, depending on surgical requirements and the animal's overall health.
In some cases, such as critically ill patients who may not be able to tolerate the side effects of inhalational anesthesia, regional Anesthesia is the only technology that can provide a complete block of pain signals to the brain without the associated heart suppression issues associated with inhalational anesthesia. An additional advantage of intraoperative antialgesia is improved anesthetic safety, as the dose of inhalant or minimum alveolar concentration required to produce anesthesia at the surgical level is reduced in patients receiving local/regional blocks as part of a multimodal analgesic regimen ( MAC) is reduced. In this article, we'll take a look at five common regional anesthetic block techniques that your practice can use to improve patient comfort, increase staff job satisfaction, and increase revenue.
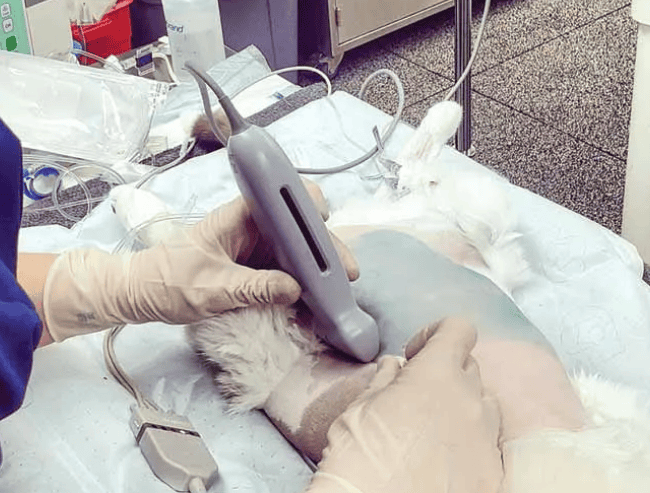
1) Transverse abdominal plane (TAP) block. This is a local anesthetic technique that involves the injection of local anesthetic into the plane of the transverse abdominal muscle, which is located between the internal oblique and transverse abdominal muscles. TAP blocks are commonly used for analgesia during abdominal surgery in dogs and cats. The procedure is relatively simple and involves placing the animal in the lateral recumbent position and determining the correct injection site. A planar ultrasound probe is used to visualize the abdominal fascial layers before surgery, and local anesthetic is injected. With this technique, the local anesthetic is distributed along the fascial layer and contacts the peripheral nerves originating from the abdominal branches of the corresponding spinal nerves. While this block does not reduce pain signals originating from internal organs, it does cover the skin and muscle layers of the abdomen. Especially when combined with a long-acting local anesthetic, TAP blocks can provide smooth recovery and long-lasting analgesia at the incision site. A 2022 study showed that a mixture of bupivacaine and dexmedetomidine administered via a TAP block provided superior postoperative analgesia compared with placebo, but was not as effective as liposome-encapsulated cloth. The analgesic level of pivacaine is the same.
2) Epidural anesthesia involves the injection of a local anesthetic into the epidural space, which is located between the spinal cord and spine. Epidural anesthesia can be used for pain relief during surgery in the pelvic area, hind limbs, or abdomen. This anesthesia can be given as a single injection or as a continuous infusion through an epidural catheter.
There are many options for placing medications in the epidural space, from preservative-free local anesthetics to opioids like preservative-free morphine. Clinicians may choose to use an opioid-only epidural to provide superior analgesia while preserving motor function. It is important to note that all medications entering the epidural space should be preservative-free.
The use of epidural anesthesia is very common in many surgeries, such as cesarean section. For those facilities that perform emergency cesarean sections, having staff who are trained and proficient in epidural anesthesia can improve overall patient safety because less inhalational anesthetic is used, which can cause vasodilation and decreased cardiac output). However, epidural anesthesia does require a certain level of skill and training, but there are now many options for hands-on training, with many major conferences offering training courses such as wet labs.

3) Sacrococcygeal nerve block. As one of the less widely used regional analgesic techniques, sacrococcygeal nerve block is suitable for patients with severe urethral obstruction who urgently need analgesia but whose critical condition cannot use narcotics or sedatives that may cause hypotension, bradycardia, or arrhythmia. In other words, it can be said to be life-saving. A sacrococcygeal nerve block involves injecting a local anesthetic into the nerves supplying the tail region. This method is commonly used to provide analgesia for urethral obstruction, but is also useful in patients with tail amputations, anal sac resections, and perineal urethrostomy. This procedure involves locating the space where the end of the sacrum meets the first coccyx vertebra and injecting a local anesthetic there. A sign of a good block is complete loss of anal tone and the penis relaxing enough to exit the foreskin, helping to facilitate urinary catheterization. Sacrococcygeal nerve block has its advantages compared to epidural block in that the motor function of the animals' hind limbs is preserved and they can move easily.
4) Dental block anesthesia. Not only is this one of the best ways to provide pain relief to patients undergoing tooth extraction, it is also safer and more cost-effective than using higher concentrations of inhaled anesthesia. Dental patients are often older and have multiple co-morbidities that preclude the use of certain medications, such as alpha-2 adrenergic agonists (e.g., dextromethamine) that may cause bradycardia, or benzothiazines that may cause hypotension. Azine sedatives (such as chlorpromazine hydrochloride). It is important to remember that inflamed gum tissue may have a higher pH, which may affect the time it takes for the local anesthetic medication to take effect. Some doctors buffer local anesthetics with sodium bicarbonate to help relieve the pain response caused by low pH.
However, a meta-analysis of human dental patients showed no benefit from adjusting the pH of lidocaine. Adjusting the pH of lidocaine did not effectively reduce pain during intraoral injections into normal or inflamed tissue. The use of buffered lidocaine did not improve the onset time of anesthesia in normal tissue. As always, knowledge of anatomy and foramen/nerve location are required when performing dental blocks including, but not limited to, infraorbital nerve blocks, maxillary nerve blocks, mental nerve blocks, and mandibular nerve blocks. training is essential.

 扫一扫微信交流
扫一扫微信交流
发布评论